Cancer Gene Therapy
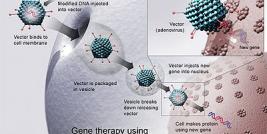
Replication-defective adenoviruses are widely used as gene transfer vectors to deliver cytostatic or tumour suppressor genes into a variety of cancers, yielding some of the most promising results in the clinic. Indeed, the most successful adenoviral vectors used to date are those that are designed to deliver p53 into tumours. Tumor cells have lost the function of p53 because of mutations in the DNA-binding region of the molecule, a feature that is present in over 50% of all human malignancies. A number of studies have demonstrated that transfer of wild type (wt) p53 gene is able to suppress tumor cell proliferation. Moreover, platinum-based chemotherapy enhances mutations in the p53 in the heterogenous cell population; transfer of the wild type p53 gene enhanced the sensitivity of chemoresistant cells to cisplatin and cisplatin-induced apoptosis (Kigawa et al, 2002). This has led to a significant amount of clinical trials where wt p53 has been re-introduced to tumour cells by the use of first-generation adenoviral vectors.
In one such study, the long-term follow-up of heavily pretreated patients with recurrent ovarian cancer by p53 gene replacement was followed by multiple cycles of platinum-based chemotherapy (Buller et al, 2002a,b). The median survival of individuals who received multiple doses of the adenoviral p53 with chemotherapy was 12-13.0 months, compared to only 5 months for those treated with a single-dose of adenoviral p53; this compared favorably to the 16-month median survival for individuals treated with paclitaxel at the time of initial recurrence of this disease and was more than double the 5-month survival seen with palliative radiotherapy or paclitaxel failure. In spite of adenoviral-induced inflammatory changes, intraperitoneal adenoviral p53 treatment was safe as a 5-day regimen using 7.5 x 10(13) adenoviral particles per dose per day followed by intravenous carboplatin/paclitaxel chemotherapy and resulted in a significant reduction of the serum tumor marker CA125 (Buller et al, 2002a,b). The results from this study demonstrate that if gene therapy of cancer is to be successful, it is important that effective combinatorial approaches are employed.
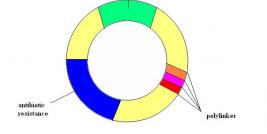
The wealth of clinical data available on adenoviral-p53 gene transfer in cancer patients led to the approval of one such product, Gendicine, for use in SCHNN by the Chinese State FDA in 2003. Gendicine comprises a recombinant adenoviral vector expressing p53 under control of a constitutively active viral promoter, in this case that of the rous sarcoma virus, and is used in the treatment of both SCCHN and NSCLC. Gendicine is produced by the Chinese company, Shenzhen SiBiono GeneTech and has been administered to over 2500 patients to date. It has been well tolerated by patients, with no serious adverse events reported; in general the only side effect seen is a Grade I-II self-limited fever. This bodes well for companies developing anti-cancer gene therapy products in the West, especially for Introgen Therapeutics, Inc., who have developed and almost identical treatment to Gendicine. As the number of patients receiving Gendicine increases (including a number of westerners travelling to China for treatment) and positive case studies continue to be documented, Western regulatory bodies may find themselves under pressure from patient support groups to open up this type of treatment for their own populations.
The Introgen product, Advexin, initially developed by the University of Texas is an example of one of the earliest cancer-specific gene therapy agents developed, with the initial clinical trials taking place in 1995. It is also, perhaps, one of the most promising cancer gene therapeutics evaluated to date. A series of phase I/II clinical trials, in a number of different indications, demonstrated that the virus was well tolerated and could mediate efficient expression of p53 in tumor cells. In 2003, Advexin was granted orphan drug status by the FDA, for the treatment of Head and Neck cancer, and was subsequently fast-tracked for approval in this indication. Since then Introgen has streamlined its Advexin clinical studies and is currently focussing its activities on two ongoing phase III trials, where Advexin is administered to Head and Neck cancer patients, with or without adjuvant methotrexate or cisplatin/fluorouracil treatment. More recently, Introgen has incorporated the use of a predictive mutant p53 biomarker test into these trials, in an effort to determine which patients may respond to the therapy. Results from the phase II studies in SCCHN, Li-Fraumeni Syndrome, lung and prostate cancers indicated that all the 35% of patients who responded to Advexin tested positive for an abnormal p53 biomarker. This should go some way to help convince the FDA that Advexin is a viable therapeutic option for SCCHN, especially if candidate patients can be pre-selected using this new prognostic test.
References
Buller RE, Shahin MS, Horowitz JA, Runnebaum IB, Mahavni V, Petrauskas S, Kreienberg R, Karlan B, Slamon D, Pegram M: Long term follow-up of patients with recurrent ovarian cancer after Ad p53 gene replacement with SCH 58500. Cancer Gene Ther 9: 567-72, 2002.
Buller RE, Runnebaum IB, Karlan BY, Horowitz JA, Shahin M, Buekers T, Petrauskas S, Kreienberg R, Slamon D, Pegram M: A phase I/II trial of rAd/p53 (SCH 58500) gene replacement in recurrent ovarian cancer. Cancer Gene Ther 9: 553-66, 2002.
Kigawa J, Sato S, Shimada M, Takahashi M, Itamochi H, Kanamori Y, Terakawa N (2002) p53 gene status and chemosensitivity in ovarian cancer. Hum Cell 14, 165-171.