Article by: Yi Lu
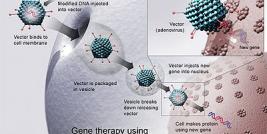
Prostate cancer is the most frequently diagnosed cancer and the second leading cause of cancer deaths in American males today. Novel and effective treatment such as gene therapy is greatly desired. Gene therapy is the direct transfer of DNA into patients’ diseased cells for the purpose of therapy. Viral based gene therapy is to use a genetically-modified, replication defective or so-called cold virus as the gene transfer vehicle. In contrast, nonviral gene therapy is to deliver DNA by nonviral methods. At the current stage, viral gene therapy in general has a much higher gene transfer efficiency in vivo compared to nonviral gene therapy. The early viral-based gene therapy uses tissue-nonspecific promoters, which causes unintended toxicity to other normal tissues. In this mini-review, we will focus on discussion of strategy using transcriptionally-regulated gene therapy strategy for prostate cancer treatment.
Comparison of different delivery routes
Theoretically, metastatic disease may only be treated by the systemic delivery of gene vectors. However, for locally advanced prostate cancer, variations in delivery strategy may help to target gene therapy vectors to the prostate. We have conducted a study of comparison of effectiveness of gene transfer by adenoviral vectors to the prostate by three different delivery routes in a canine model (1). An adenoviral vector (AdRSVlacZ) expressing bacterial E.coli ß-galactosidase (lacZ) reporter gene under the control of a constitutively active Rous sarcoma virus (RSV) promoter was administrated by intravenous, intra-arterial (inferior vesical/prostatic artery), and intraprostatic injections. Seventy-two hours after injections, the expression of the lacZ gene was measured in canine prostate and various other organs by in situ X-gal staining and ß-galactosidase enzymatic activity of tissue extracts. The distribution of the disseminated adenoviral vector was determined by PCR of genomic DNA using primers specific for adenoviral genome. The study showed that intraprostatic injection of adenoviral vector resulted in a greater transduction rate and expression level of lacZ in the prostate than either intravenous or intra-arterial injection. Thus, intraprostatic (or intratumoral) injection seems to be the best route to treat local regional prostate cancer by viral based gene therapy. It is not surprising therefore that most gene therapy clinical trials for patients with prostate cancer have administrated vectors into the prostates/tumors (2, 3, 4, 5, 6, 7, 8, 9, 10).
Study of transcriptionally regulated, prostate-targeted viral vectors
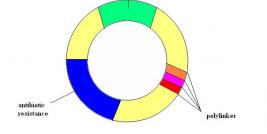
The early viral based vectors for gene therapy are mostly tissue nonspecific because of constitutively active viral promoters such as cytomegalovirus (CMV) and rous sarcoma virus (RSV) promoters. Consequently, the expression of the delivered therapeutic gene may occur in unintended, nontargeted tissues which may potentially cause systemic toxic effects, especially if a toxic gene is the expressed gene. To minimize systemic toxicity of adenoviral-mediated toxic gene therapy, prostate specific promoters have been used in attempt to allow the exclusive expression of the therapeutic gene in the prostate.
Several prostate tissue specific promoters have been defined over the years that include promoters of prostate specific antigen (PSA), probasin (PB), mouse mammary tumor virus (MMTV LTR), prostate specific membrane antigen (PSMA), human glandular kallikrein-2 (hK2) and prostatic steroid-binding protein C3. The PSA promoter has an androgen response element (ARE) and its activation requires both the androgen receptor (AR) and its ligand, androgen, to be present. Recently, the promoter of PCAN1, a newly discovered gene with remarkable prostate tissue specificity, has been demonstrated to be a promising candidate for regulating prostate specific gene expression with high-level activity.
We have constructed adenoviruses that contain a bacterial ß-galactosidase (ß-gal) gene (lacZ) under the control of three different prostate-specific promoters: PSA, probasin, and MMTV (prostate-specific Ad-lacZ). In general, these prostate-specific Ad-lacZ can effectively transduce and express ß-gal in prostate cells and had no or weak expression of ß-gal in non-prostate cells in vitro. In vivo, these adenoviruses had a high level of ß-gal expression in canine prostate, but also disseminated to tissues other than prostate after intraprostatic (i.p.) injection. However, none of the prostate-specific Ad-lacZ expressed ß-gal in these non-prostate tissues (11,12). Furthermore, prostate-specific Ad-lacZ only expressed ß-gal in xenograft tumors grown in nude mice derived from human prostate cancer cells, DU145 and PPC-1, and not in tumors derived from human bladder cancer cells, RT4. These results indicate that adenoviruses containing prostate specific promoters may express intended transgenes specifically in prostate in vivo (12,13).
Selection of therapeutic strategies for prostate cancer gene therapy
The choice of therapeutic transgenes and gene therapy strategies are rapidly evolving with the advances in identification of new genes and new targets, improvement of vectors and expression systems, and better understanding of molecular biology of prostate cancer. The choice of the therapeutic transgenes usually determines the therapy strategies. The gene therapy strategies for prostate cancer can be mainly categorized as: (i) corrective gene therapy, (ii) programmed cell death gene therapy, (iii) suicide gene therapy including the gene directed enzyme prodrug therapy (GDEPT), (iv) immunomodulation therapy, (v) conditional oncolytic virus approach (see more below), although sometimes it may appear difficult to define a therapeutic gene or strategy into one category due to its relevance to both categories (a good example is tumor suppressor gene p53 that fits both the first two categories). The strategy in category (i), (ii) and (iii) can be combined with a prostate-specific promoter to render a tissue-specific regulated expression of therapeutic transgenes.
Oncolytic virotherapy for prostate cancer
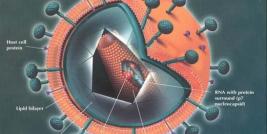
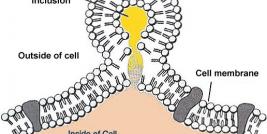
The adenovirus early region 1 (E1) gene, which comprises E1a and E1b, encodes the viral early proteins that are necessary for adenoviral replication and the consequent oncolysis of permissive host cells. E1-deleted adenoviruses are replication-defective and are commonly used as viral vectors to carry therapeutic genes for gene therapy. E1-deleted viruses infect host cells and express the transgene but they cannot replicate and undergo lysis due to the lack of the E1 protein. Thus, E1-deleted recombinant adenoviruses are a safe viral vehicle for gene transfer. However, E1-deleted, replication-defective adenoviruses have several common problems with respect to in vivo transduction: a low transduction rate, time-limited expression of the transgene, and host immune responses to repeated viral administration.
Virotherapy is a bold yet logic strategy that employs conditional oncolytic virus, or so-called attenuated replication-competent virus, for cancer gene therapy. Because oncolytic virus replicates in the transduced cells and enters lysis cycle, the lyzed virus infects the neighboring cells and continues this cycle until all the cells are eliminated, theoretically a large burden of tumor can be effectively eradicated by a small dose of oncolytic virus. The key issue to use this strategy is the “conditional” oncolytic virus, that is, the virus is altered to specifically target desired cell type or attenuated in a way that the desired target cells are much highly sensitive (in several magnitude differences) to its oncolytic cell lysis than nontargeted cells.
By taking advantage of prostate-specific promoter, an Ad5 E1a gene, whose product allows adenovirus to replicate and to enter the lytic cycle, was reintroduced to E1a/E3-deleted adenovirus under the control of PSA enhancer/promoter (-5322 to –3729/-580 to +12) (PSE). The resultant adenovirus, CN706, specifically replicates in and thus kills PSA-producing cells such as LNCaP but not PSA-non-producing cells such as DU145 (14). Likewise, adenoviral vector CN764, that contains PSE, driving the Ad5 E1a gene, and the hK2 enhancer/promoter (-5155 to –3387/-324 to +33), driving the Ad5 E1b gene, significantly attenuates in the primary human microvascular endothelial cells. It has a high therapeutic index with a cell specificity of 10,000:1 for prostate cancer LNCaP cells, compared to ovarian cancer OVCAR-3, SK-OV-3 and PA-1 cells (15). By a similar approach, another prostate-specific replication-competent adenovirus, CV787, was constructed. CV787 contains PB promoter driven E1a gene and PSE driven E1b gene, plus a wild-type E3 region that suppresses host immune system. CV787 destroys PSA-producing cells 10,000 times more efficiently than PSA-nonproducing cells. A single tail vein injection of CV787 eliminates distant LNCaP xenograft tumors (16), indicating that it has the potential to be developed as a powerful therapeutic vector for metastatic prostate cancer.
Summary
The current treatments for prostate cancer include surgery, radiation therapy, hormone therapy (androgen deprivation), chemotherapy, and gene therapy. It is most likely that gene therapy may have the best potential for prostate cancer treatment when in conjunction with other therapeutic modality. There are currently 23 NIH-approved clinical trials (including active, recruiting, and recently completed trials) on prostate cancer gene therapy (www.clinicaltrials.gov). The completed trials for localized prostate cancer include strategies of GDEPT suicide gene therapy (4), oncolytic virotherapy (3), immunotherapy (10), combined suicide gene therapy with radiotherapy (2), and combined suicide gene therapy with virotherapy and radiotherapy (8, 9). The majority of these trials used adenoviral vectors and almost all of them exclusively applied intraprostatic injection for gene delivery (17). Although positive PSA responses, a surrogate endpoint for prognosis, were observed in these trials, the vast majority of responses were short-lived, reflecting a lack of sustained therapeutic efficacy. On the other hand, the completed trials for metastatic prostate cancer include strategies of transcriptionally-regulated GDEPT suicide gene therapy (18), transcriptionally-regulated oncolytic virotherapy (19), vaccine therapy (20, 21, 22, 23, 24, 25, 26, 27), or a combination of vaccines and immunotherapy (28). While they all present an encouraging, short-term low toxicity, the therapeutic efficacies are not ideal and still need to be improved.
In summary, the success in gene therapy for prostate cancer will rely on the advances in vector system and delivery strategy, exploration of new targets and therapeutic genes, better understanding of biology of prostate cancer, and invention of more clinically relevant animal models for human prostate cancer. With its gradual trial and success in the treatment from localized prostate cancer to metastatic prostate cancer, gene therapy, especially the transcriptionally regulated, prostate-targeted strategy, may represent a new avenue for the development of multi-modal treatments for advanced prostate cancer.
Dr. Yi Lu is an Associate Professor at the Department of Pathology and Laboratory Medicine, University of Tennessee Health Science Center, Memphis, TN, USA.
CORRESPONDENCE: Yi Lu, Ph.D. Department of Pathology and Department of Medicine University of Tennessee Health Science Center Cancer Research Building, Room 218 19 South Manassas Street Memphis, TN 38163, USA Telephone: (901) 448-5436 Fax: (901) 448-5496 e-mail: ylu@utmem.edu