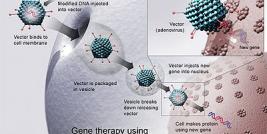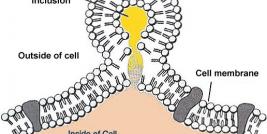
Cancer can be described as a disease where cellular communication has broken down, allowing transformed cells to escape tight regulatory signals and to replicate autonomously and continously, ultimately invading and interfering with the functions of normal tissues. Under physiological conditions cells communicate with one another by activating receptors at the cell surface, which convey the signal through pathways of proteins located in the cytoplasm and subsequently through networks of transcription factors in the nucleus with control the expression of genes that mediate the cell's response. In this article we briefly describe the gene therapy approaches that have been adopted in an effort to treat cancer.
Typically, cancer develops as a result of aberrant growth factor signalling, where a pathway that instructs a cell to grow and divide becomes constitutively active. This arises through mutations in a growth factor receptor, or through mutations in the components of cell signalling pathways. (Collectively, genes that encode for mutated cellular proteins involved in promoting cell growth are termed oncogenes). Threrefore, in order to effectively treat a cancer, it is essential that all cells that carry a mutated oncogene, are destroyed, otherwise the cancer will continue to grow and spread.
Cancer Gene Therapy Approaches
There are a number of gene therapy-based clinical trials in the field of oncology currently underway worldwide, encompassing a variety of delivery agents, target indications and means of intervention. All therapeutic strategies that are being developed in the treatment of cancer ultimately aim to destroy cancerous cells whilst leaving normal cells unaffected. This can be achieved by using one (or more) of the following approaches:
i. Expression of tumour suppressor genes
In many types of cancer, deactivating mutations arise in specific genes whose function is to prevent the uncontrolled growth of the cell. Genes that regulate cell division in this manner are called tumour suppressor genes (TSG); two examples include p53 and Rb. It has been found that re-introduction this type of gene into cancer cells initiates a series of events that results in the ultimate death of the cancer cell. Moreover, because normal cells of the body have the correct copy of these genes, the expression of a TSG in normal cells has no significant pathological effects. Therefore, it is generally considered that TSG expression in tumours is a safe way to specifically kill the cells that comprise the cancer. The only state-approved gene therapy treatment adopts this type of approach and is used in the treatment of both lung cancer and squamous cancer of the head and neck. This drug, called gendicine (gene medicine) and comprises an adenovirus expressing p53, was registered by the Chinese State Food and Drug Administration (SFDA) in 2003 and has been successfully used in the treatment of these two cancers, specifically when administered in conjunction with traditionally used chemotherapeutics.
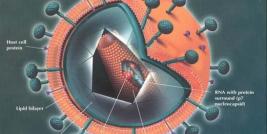
ii. Oncolytic viruses
For almost a century it has been known that certain types of virus can kill cancer cells if they are induced to replicate inside them. Research is currently being conducted by institutions around the world using both "non engineered" and "engineered" viruses to evaluate their use in the fight against multiple types of cancer. Non engineered viruses are naturally occurring viruses that innately preferentially target and replicate in certain types of tumor cells. Some non-engineered viruses include the Newcastle Disease Virus, Autonomous Parvovirus, and the Reovirus. Conversely, engineered viruses do not innately selectively target and replicate in cancer cells. Scientists must genetically modify ("engineer") the virus to selectively target and/or replicate within specific types of cancer cells. Today, there are three main approaches that are being explored in the development of engineered tumor-specific oncolytic viruses. Although the three approaches differ from one another, they all share a common goal—the destruction of cancer cells as a result of viral replication. The three approaches are as follows:
1. Selective Targeting—Capsid Protein Modification: The capsid protein, the external surface of the virus, is modified so that the virus will specifically target cancer cells, completely avoiding normal cells. The virus would then replicate within the targeted cancer cell, ultimately leading to cell death.
2. Selective Replication in the Absence of an Antitumor Gene: The virus is genetically modified so that it will replicate only in the absence of a gene believed to inhibit tumor cell growth, such as P53. While the virus "passes through" normal cells, it is triggered to replicate in cancer cells that do not exhibit an antitumor gene, ultimately leading to cancer cell death.
3. Selective Replication in the Presence of Unique Tumor Cell Characteristic:
The virus is genetically modified so that it will replicate only in the presence of a characteristic (e.g. an antigen) unique to the specific type of cancer. While the virus passes through normal cells, it is triggered to replicate in cancer cells that exhibit a specific characteristic, ultimately leading to cancer cell death. Cell Genesys' oncolytic virus product platform utilizes this approach.
Research and development efforts are currently under way at numerous organizations to thoroughly evaluate the safety and efficacy of oncolytic virus therapies. The majority of the studies currently being conducted are utilizing intratumoral delivery of the oncolytic virus therapies. Direct administration into the tumor allows the oncolytic virus immediate "access" to the cancer cells in which they replicate and ultimately destroy. Additional studies are being conducted to determine the safety and efficacy of intravenous administration of oncolytic virus therapy. While intravenous administration holds the promise of providing systemic treatment and targeting cells that have spread from the primary tumor source, researchers are faced with the challenge of maintaining therapeutic levels of the virus in the presence of the immune system which intrinsically seeks to rid viruses from the body. Intravenously administered oncolytic virus therapy must overcome pre-existing antibodies in order to achieve therapeutic effect. Alternatively, research is being conducted to determine a way to modulate the immune response allowing the virus time to reach the primary tumor source as well as target cancer cells that have spread throughout the body.
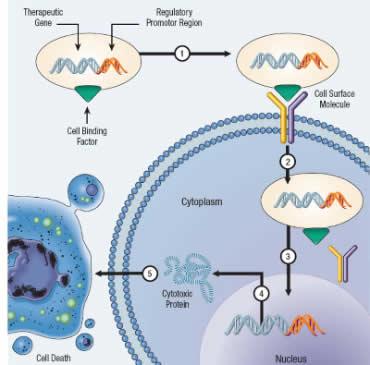
iii. Expression of genes that initiate cell death
Programmed cell death, known as apoptosis, is an essential cellular homeostasis mechanism that ensures correct development and function of multi-cellular organisms. The pivotal importance of correct execution of apoptosis is apparent from the many human diseases with aberrancies in apoptosis, including cancer. During cancer development, various imbalances can arise in the apoptotic machinery. Consequently, sensitivity towards apoptosis is progressively reduced, which ultimately leads to inappropriate cell survival and malignant progression. However, it has become clear that cancer cells are often reliant on these aberrancies for continued survival. Perhaps counter intuitively, cancer cells can in fact be more prone to apoptosis than normal cells. The apoptosis-prone phenotype of cancer cells is masked and counterbalanced by upregulation of one or more anti-apoptotic mechanisms. Therefore, it is of enormous therapeutic interest to selectively tip the balance of the cellular fate of cancer cells towards apoptosis. Gene therapy can be employed to exploit this weakness in cancer cells by using recombinant gene transfer vectors to express genes that promote programmed cell death. These can either be the ligands that activate death receptor signalling, or the components of the apoptotic machinery that mediate these signals. At present there are a wealth of clinical trials underway that exploit the sensitivity of cancer cells to pro-apoptotic signals and it represents an emerging sub-field within the gene therapy arena.
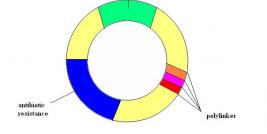
iv. Gene-directed enzyme pro-drug therapy
In this approach tumour cells are killed by the specific action of a toxic drug that is produced from a non-toxic precursor by the action of an activating enzyme. In the clinical setting, an appropriate vector (typically viral) is first used to achieve expression of a prodrug-activating enzyme inside tumour cells. A nontoxic (or minimally toxic) prodrug is then administered and is converted to the active, toxic metabolite in cells expressing the activating enzyme. These cells are subsequently killed. Moreover, untransduced cells might also be killed following prodrug activation, by mechanisms that include direct transfer of activated drug through gap junctions, ingestion of apoptotic bodies from killed cells, effects on tumour vasculature, or immunological responses.
v. Immunotherapy
Immunotherapy is used to stimulate the body's immune system against cancer. This can be achieved in many different ways. One example is the use of vaccines composed of antigens derived from tumor cells to boost the body's production of antibodies or immune cells (T lymphocytes) to fight the cancer.Typically in this approach, gene transfer vectors are used to deliver cancer antigens to the immune cells, either by engineering the patients own T lymphocytes out of their body and re-administrating them, or by simple injection of the gene transfer vectors encoding the antigens so that the patients immune cells become infected in vivo. In a second example, a patients anti-tumour immune response can be boosted by the administration of cytokines (natural chemicals in our body that control our immune system) or antibodies that function to specifically attack cancer cells and stimulate the immune system to destroying the tumour. Immunotherapy is a huge field in its own right and is outwith the scope of this website. Readers can find more information on this topic by following the following link.