Hua Su, Assistant Professor, Center for Cerebral Vascular Research, Department of Anesthesia and Perioperative, University of California, San Francisco
My current researches are focused on developing strategies for angiogenic gene and and cell Therapies for myocardial infarction and ischemic brain injuries.
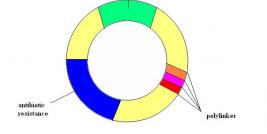
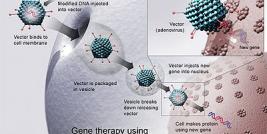
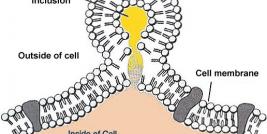
Rapid, efficient overexpression of angiogenic growth factors in the peri-infarct zone is a promising approach for gene therapy of acute myocardium infarction. We have developed an adeno-associated viral vector (AAV), AAV-MLC, that mediates cardiac-specific and hypoxia-inducible gene expression in mouse ischemic hearts model. We have also found in mouse model that by direct injection, AAV serotype 1 infect cardiomyocytes more effectively than AAV serotype 2 to 5; co-expression of angiopoietin-1 (Ang-1) with vascular endothelial growth factor (VEGF) enhances VEGF angiogenic effect and reduces VEGF mediated vessel leakage. However, the information derived from small animal models may not be directly applicable to human therapy. We are now testing whether AAV1-MLC vector can function similarly in pig model as in mouse model.
Irreversible myocardial-injury occurs shortly after coronary occlusion. Angiogenic therapy can reduce post-infarct remodeling and improve cardiac function, but it has little effect on repairing existing scars. Transplantation of stem cells from various sources into infarcted heart can repair infarct scars by direct differentiation into cardiac cells or by promoting endogenous stem cell mobilization and proliferation. However, the survival rate of transplanted cells is poor in ischemic myocardium. Combining cell therapy with gene therapy might improve the cell survival. We are currently studying the feasibility of modifying bone-marrow-derived mesenchymal stem cell (MSC) to express angiogenic factors to improve MSC mediated therapy for myocardial infarction.
Brain ischemia occurs in many brain injuries and diseases. The innate angiogenesis in response to brain injury is not sufficient to prevent tissue damage caused by ischemia. However, to induce angiogenesis by delivery exogenous angiogenic genes apposes a number of particular challenges, including: a) a necessity for intact barrier function; b) a specific temporal window; and c) the localization of the pro-angiogenic signal to areas of injury. We are testing the feasibility of using AAV mediated hypoxia-inducible angiogenic gene expression to induce angiogenesis at ischemic core/penumbra in ischemic brain and co-expression of VEGF with anther angiogenic factor to enhance angiogenesis and reduce leakage of brain blood barrier. We are testing the feasibility of using human stem cell derived oligodendrocytes to regenerate injured brain. We are also studying the roles of micro RNA in neuron stem cell differentiation, migration and in brain injuries.