Article by: Ethan Y. Yang and Hua Su
Hua Su holds a position at the UCSF Eli and Edythe Broad Center of Regeneration Medicine and Stem Cell Research, where she is a professor working on angiogenic gene and cell therapies for ischemic cardiomyopathy and stroke.
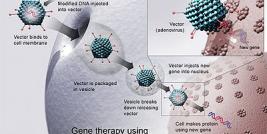
Prolonged ischemic insult can cause irreversible tissue injuries. Despite advances in medical and surgical therapies, myocardial infarction and stroke, both consequences of ischemic insults, remain to be the top two causes of morbidity and mortality in the Western world, with survivals usually carrying permanent disabilities. Treatments that help restoring blood flow to ischemic area remain to be one of the most important therapeutic goals. Enhancing the innate angiogenesis by exogenous delivery of angiogenic factors lessens the ischemic injury. However, uncontrolled angiogenic gene expression can cause some unwanted side effects. In this mini-review, we describe two systems that can be used to mediate hypoxia-inducible and tissue-specific gene expression.
Recent studies have shown that enhancing the innate response to ischemic injury by exogenous delivery of angiogenic factors promotes a certain degree of functional recovery. Endogenous secretion of these factors is inadequate, while unregulated gene expression can cause some unwanted side effects, such as hemangioma formation at injection sites (1). Examples of inducible promoters that have been used to control gene expression include tetracycline operons, RU 486, edyasone, and other inducible systems. However, these systems require the exogenous administration of an inducer to enhance expression of the therapeutic gene, which may not applicable in patients.
Intrinsic hypoxia activates hypoxia inducible factor-1 (HIF-1), which upregulates down–stream angiogenic factors, resulting in focal angiogenesis (2, 3). Previous experiments have shown that HIF-1? level increases in ischemic myocardium beginning two days after occlusion of the left anterior descending coronary artery (LAD) (4). HIF-1 is also greatly increased in the ischemic brain at four hours after middle cerebral artery occlusion (MCAO) (5). Thus, hypoxia-induction of angiogenesis is an ideal system where gene expression can be promoted expediently in ischemic heart or brain.
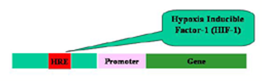
Figure 1. Schematic drawing shows hypoxia-inducible system. HIF-1 protein will accumulate in ischemic tissues and bind to hypoxia response elements (HREs) sequence in the enhancers of genes, which will lead to up-regulation of downstream genes.
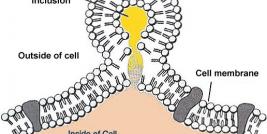
Hypoxic induction of gene expression through activation of HIF-1 is one of the major mechanisms to regulate gene expression in response to hypoxia stress. This system consists of an enhancer element, hypoxia-response element (HRE), and the transactivating factor, HIF-1 (Figure 1). HIF-1 is a protein that accumulates in tissues under hypoxic conditions. This protein is a heterodimeric basic helix-loop-helix protein and has a labile alpha subunit (HIF-1alpha) and an alpha subunit (HIF-1alpha). The alpha subunit is constitutively expressed in tissues in normal and hypoxic conditions. HIF-1alpha protein is rapidly degraded via ubiquitination and proteasomal digestion. HIF-1alpha degradation is mediated by a 200 amino acid oxygen-dependent degradation domain. This subunit is stabilized in hypoxic tissues and binds to the alpha subunit to form functional HIF-1 protein that activates transcription of several genes, including erythropoietin (Epo) and vascular endothelial growth factor (VEGF) genes, in hypoxic cells through binding to hypoxia-response elements (HREs) in their enhancers (Figure 1). Together, HIF-1, Hepatocyte Nuclear Factors (HNF1, HNF4) bind to HRE regions of Epo to maximize hypoxia-induced gene expression (Figure 2).
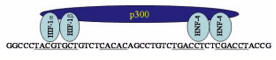
Figure 2. Elements and factors that regulate hypoxia induction of gene expression. Multiprotein complex containing hypoxia-inducible factor 1, an adjacent transcription factor (HNF-1 for Epo gene), and p300/CREB binding protein together maximize hypoxia-driven gene expression
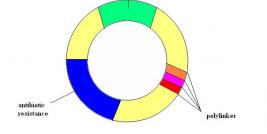
Hypoxia-inducible gene expression can also be encouraged by using multiple copies of HRE consensus sequence in combination with a promoter with minimal promoter function (Figure 3). It has been demonstrated that four or nine copies of HRE isolated from human erythropoietin enhancer and a minimum SV40 promoter can mediate VEGF and LacZ gene expression in both ischemic myocardium and brain (4, 6, 7).
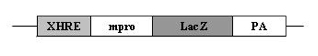
Figure 3. Schematic drawing of an expression cassette with X copies of Epo HRE (XHRE) cloned in front of promoter sequence with minimum promoter function. The expression of LacZ gene mediated by this expression cassette is hypoxia inducible.
Tang and colleagues have designed a vigilant plasmid system to encourage hypoxia-inducible gene expression (8). It is a double-plasmid system that consists of a sensor plasmid that has a promoter and an oxygen-sensitive toggle (OST), and an effecter plasmid that express protective genes. In the sensor plasmid, the biosensor is derived from the oxygen-dependent degradation domain (ODD) (amino acids 394–603) of HIF-1alpha. The ODD was inserted in the frame between the coding sequence of the GAL4DNA binding domain and the p65 activation domain (P65AD). When activated by low oxygen, the sensor plasmid expresses a fusion protein (GAL4-ODD-P65AD) that is stable and migrates to bind to the upstream activating sequence (UAS) of the effecter plasmid. Finally, the gene in effecter plasmid is driven by six copies of a 17-bp GAL4 UAS and an adenovirus-derived E1b TATA box.
Both of these systems induce gene expression in ischemic tissues within hours after hypoxia, which fit with the treatment time window for sub-acute or chronic ischemia. The double-plasmid system described gives a much more potent and optimal physiological control of HRE-mediated expression under hypoxia, rendering transgene expression increase up to 400 fold (8). However, in order to achieve specific gene expression, 2 vectors have to be introduced into the same cell. The single vector system mediates relatively lower level of gene expression, which may help circumvent side effects caused by high level gene expression. This vector system can be modified to combine tissue-specific promoters, such as cardiac-specific myosin light chain 2v (MLC-2v) promoter for heart, to mediate tissue specific and hypoxia-inducible gene expression (8, 9).
Angiogenic gene therapy has been studied as an option for the treatment of hypoxia and ischemia tissue injuries. However, uncontrolled gene expression can cause some unwanted side effects, such as hemangioma formation. The above methodologies provide tools for regulation of transgene expression that will lead to development of safe gene therapy strategies for the treatment of ischemic diseases.