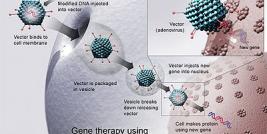
Gene Therapy Strategies for HIV-1 Treatment
Human immunodeficiency virus (HIV) is the causative agent of acquired immunodeficiency syndrome (AIDS) [1]. According to the report from World Health Organization (WHO), in 2009, there were 33.3 million people living with HIV/AIDS, with 2.6 million new infections and 1.8 million deaths due to AIDS (http://www.who.int/hiv/data/2009_global_summary.png). HIV infection affects a large area and spreads actively ever since it was identified, with a significant number of AIDS deaths occurring in Sub-Saharan Africa [Greener R (2002) AIDS and macroeconomic impact. In S, Forsyth (ed) State of the Art: AIDS and Economics IAEN: pp. 49-55].