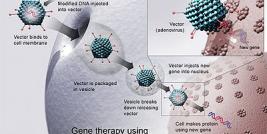
New avenues of research are constantly needed to establish experimental and therapeutic protocols that may lead to a better understanding and management of major human diseases. Gene-based approaches are promising tools to achieve these goals, in particular those based on the use of recombinant adeno-associated virus (rAAV) vectors as vehicles for candidate gene sequences. In the Laboratory for Experimental Orthopaedics (Department of Orthopaedic Surgery, Saarland University Medical Center, Homburg/Saar, Germany), we are developing since some years molecular approaches based on the generation of rAAV vectors as tools to provide insights into key pathological processes and as therapeutic options against diseases where no treatments are available, including disorders of the musculo-skeletal and nervous systems.
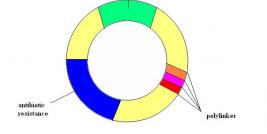
Regarding the musculo-skeletal system, the potentiality of rAAV vectors is well-known, as transduction with this class of vector has been successfully achieved in several cell types (1, 2, 3, 4). In light of these observations, we examined the permissivity of articular chondrocytes to these vectors as a strategy to treat articular cartilage disorders. Articular cartilage lesions, such as resulting from trauma or osteoarthritis (OA), are a major unresolved problem for orthopaedic surgeons due to the very limited intrinsic ability of the cartilage to heal. Diverse conservative and surgical interventions are currently employed to improve the quality of the repair tissue, but none can reproduce an original hyaline articular cartilage (5). We have created new therapeutic rAAV vectors based on the use of regulators of cartilage metabolism (growth and transcription factors) using the CMV-IE promoter to achieve high levels of production of each factor. We derived these vectors from AAV serotype 2 (AAV-2) that transduces articular chondrocytes with high efficiencies. We first examined the ability of an rAAV vector encoding the human fibroblast growth factor 2 (FGF-2) to improve the repair of articular cartilage defects in vivo, as this factor has been shown to stimulate cell proliferation in vitro (6, 7) and chondrogenesis in vivo (8). The functionality of the vector was monitored in primary cultures of rabbit articular chondrocytes in vitro and in osteochondrondral defects created in the trochlear groove in the knee joints of rabbits. We demonstrated that rAAV-mediated overexpression of FGF-2 promoted the proliferation of articular chondrocytes in vitro. Direct administration of the rAAV FGF-2 vector via arthrotomy in osteochondral defects in vivo improved the structural quality of the repair tissue (9). There were no adverse reactions and no effects upon the immune system (no cell infiltration). These data demonstrate that therapeutic rAAV vectors are capable of enhancing articular cartilage repair and provide further motivation into the optimization of gene transfer approaches to treat articular cartilage defects in patients. We next evaluated the ability of an rAAV vector carrying a sox9 gene sequence to modulate the composition of extracellular matrix in human OA articular cartilage, as this transcription factor has been shown to promote the differentiation of chondrocytes (10) and the formation of articular cartilage (11). We observed that overexpression of sox9 via rAAV in isolated human normal and OA chondrocytes stimulated the synthesis of proteoglycans and type-II collagen, the two major extracellular matrix components of the cartilage (12). Direct application of the rAAV sox9 vector to human OA articular cartilage explants restored expression of these components to levels similar to those noted in normal articular cartilage, compensating for the loss of cartilage matrix in sites of cartilage degeneration (13). A combined FGF-2/sox9 gene transfer approach using two separate rAAV vectors was also tested in a similar system, showing improved therapeutic effects of each factor vis a vis single vector application (Cucchiarini et al., in press). These promising data are laying the basis for potent, direct molecular therapies against human OA.
Another problem in orthopaedics is the occurrence of meniscal tears in patients that can predispose the adjacent articular cartilage to OA (14). As a preliminary trial, we examined the potential of rAAV vectors to deliver genes to the meniscus by applying constructs carrying the lacZ marker gene to primary cultures of human meniscal fibrochondrocytes in vitro and to longitudinal defects in vivo experimentally created in the avascular zone of the medial meniscus in rabbits. In these experiments, efficient reporter activity was demonstrated in meniscal cells over sustained periods of time in vitro. Durable transgene expression was also noted in vivo, especially in cells adjacent to the meniscal tears. Next, strategies based on the delivery of therapeutic rAAV vectors revealed that overexpression of FGF-2 in human meniscal explant cultures promoted the cellular repopulation and healing of experimentally created meniscal lesions in situ, in particular in sites with poor regenerative capacity (15). These results show strong promises to treat directly meniscal injuries.
In a more recent part of our work, we have been interested in developing strategies based on the use of progenitor cells, in particular bone marrow-derived mesenchymal stem cells (MSCs). The manipulation of MSCs, as platforms to deliver candidate genes via rAAV delivery may find extensive applications to treat various human disorders that require tissue repair or regeneration (cartilage defects, OA, others). We have demonstrated that these cells could be effectively and persistently modified by this class of vector in a three-dimensional environment (aggregate cultures) that is relevant for further transplantation in experimental models of injuries in vivo. In particular, when transduced by an rAAV FGF-2 vector in established conditions, the cells could be induced towards a proper chondrocyte phenotype and in amounts that might be suitable for applications in vivo (16), confirming the value of the approach for therapeutic purposes.
Another key issue in current biomedical research is to identify reliable experimental systems that are relevant to a clinical situation in patients. Although diverse animal models are available that have advanced our knowledge of diverse human disorders, most are still limited in that they are difficult to handle and do not always reproduce the full pathology and progression of the disease. For these purposes, we manipulated rAAV vectors to create convenient models of human brain disorders including AIDS dementia, Alzheimer’s disease, multiple sclerosis, ischemia, and Creutzfeldt-Jakob disease. Among the components of the central nervous system, microglia (the brain´s resident macrophages) are a crucial cell population that control the development, growth, and function of other brain cells and are responsible for destroying infectious agents and promoting brain tissue repair. As a consequence, microglia become activated in response to various pathologic processes as those listed above. Owing to these central roles, microglia constitute a pivotal population for study in basic brain research, as well as for advancing the goal of gene therapy for brain disorders. In a work that was initiated with E. F. Terwilliger at the Harvard Medical School (Division of Experimental Medicine, Harvard Institutes of Medicine and Beth Israel Deaconess Medical Center, Boston, MA, USA), we have cloned and assembled microglia-specific rAAV vectors using tissue-specific regulatory elements such as those derived from genes encoding myeloid-specific antigens (CD11b, CD68, F4/80). The properties of these vectors were compared and contrasted against control vectors driven by the high-level, nondiscriminatory CMV-IE promoter. We constructed isogenic vectors from AAV serotypes 2 and 5, as rAAV-5 vectors appear able to deliver genes to most of the brain cell populations in contrast to rAAV-2 that transduce primarily the neurons (17, 18). Efficiencies of transgene expression were monitored using two distinct and complementary indicator genes, lacZ and the red fluorescent protein (RFP). Expression from each vector was assessed in vitro in microglia vis a vis other brain cells (neurons, astrocytes) and in a different macrophage lineage (lung alveolar macrophages). We have identified a microglia-restricted rAAV vector derived from serotype 5 and carrying the F4/80 promoter sequence that yielded the highest level of specificity in culture and exhibited the same level of selectivity in the intact brain in vivo (19), without any sign of inflammation or infiltration in the region of administration. The capability of genetically modifying microglia by direct rAAV injection in living animals with such ease may lead to new avenues of research into the etiologies of multiple brain pathologies and afford opportunities for gene therapy concepts to some of these disorders.
In conclusion, gene transfer approaches based on the use of rAAV vectors are of strong value for the development of experimental models and therapeutic regimens against various human disorders. The translation of such direct, potent gene delivery strategies in large animal models may further provide insights into the mechanisms governing pathophysiological processes and allow to elaborate efficient treatments against human disorders, leading to new gene therapy trials.